- Opening Hours
- Timing: Mon to Sat - 10 AM to 5 PM
- Address: Positron Hospital, Health Center Plot Block B Suncity, Sector 35, Suncity Township-I, Rohtak, Haryana 124001
- Call Us+123-456-78-09
- Opening Hours
- Timing: Mon to Sat - 10 AM to 6 PM
- Address: Positron Hospital, Health Center Plot Block B Suncity, Sector 35, Suncity Township-I, Rohtak, Haryana 124001
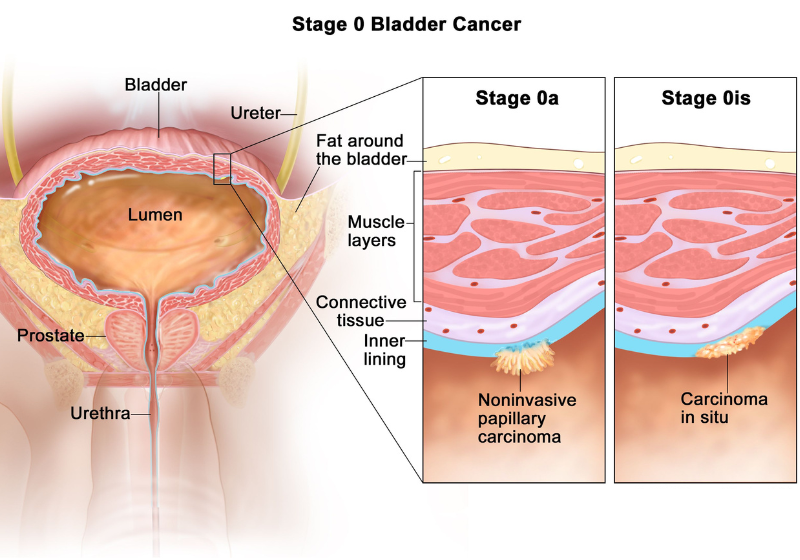
Bladder Cancer
Bladder cancer is a common malignancy that begins in the lining (urothelium) of the bladder, the organ that stores urine. It is often linked to smoking, exposure to certain chemicals, chronic bladder irritation, or infections. The most frequent type is urothelial carcinoma. Early detection is key, as most cases are diagnosed when the cancer is still confined to the bladder lining (non-muscle invasive), offering better treatment outcomes.
Common symptoms include painless blood in the urine (hematuria — visible or microscopic), frequent urination, urgency, or pelvic pain.
Diagnosis and Staging
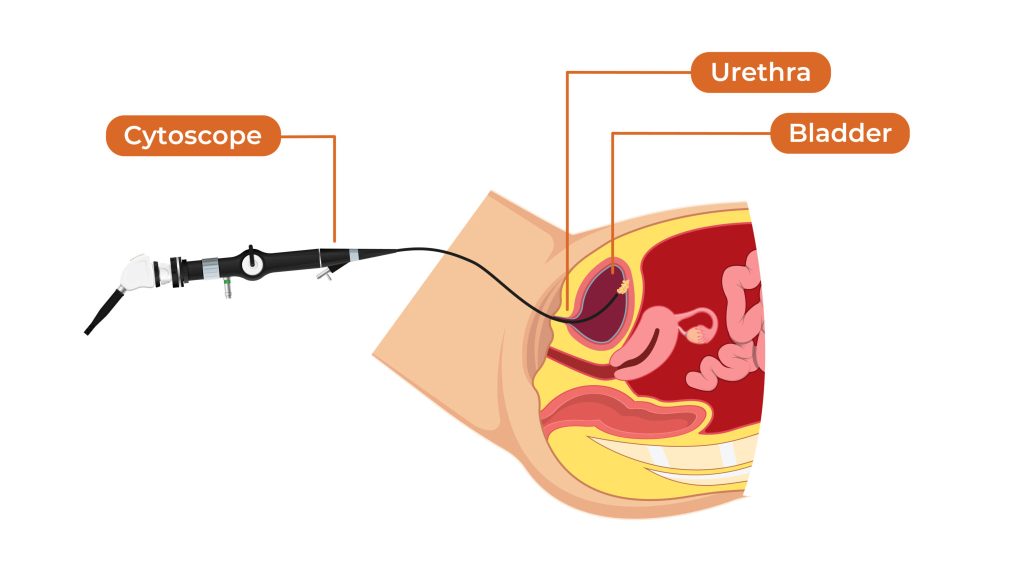
Diagnosis typically begins with urine tests (cytology, tumor markers), followed by cystoscopy — a key procedure where a thin, lighted scope is inserted through the urethra to directly visualize the bladder interior and identify tumors.
Here are visuals of cystoscopy showing a bladder tumor:
Bladder cancer is staged using the TNM system (Tumor, Node, Metastasis), from non-invasive (Ta, Tis, T1) to muscle-invasive (T2+) and advanced stages.
Treatment Approaches
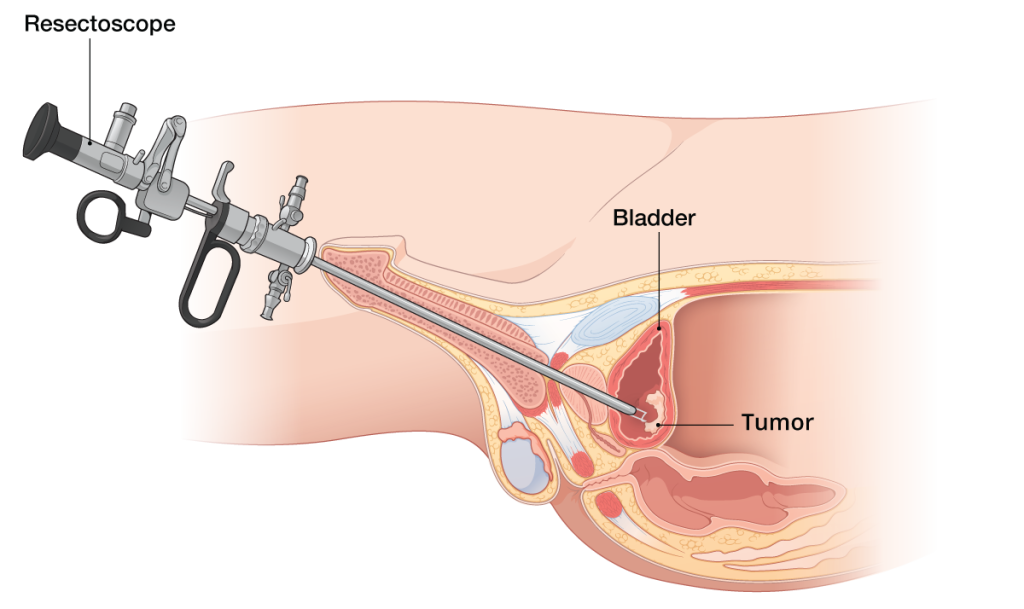
For non-muscle invasive bladder cancer, the primary treatment is transurethral resection of bladder tumor (TURBT) — endoscopic removal of the tumor through the urethra using a resectoscope.
Here are illustrations of the TURBT procedure:
After TURBT, intravesical therapy is often used to prevent recurrence: chemotherapy (e.g., mitomycin) instilled directly into the bladder, or immunotherapy with BCG (Bacillus Calmette-Guérin) for higher-risk cases.
For muscle-invasive bladder cancer, options include radical cystectomy (bladder removal with urinary diversion), chemotherapy, radiation, or bladder-preserving approaches (trimodality therapy). Advanced cases may involve systemic immunotherapy or targeted therapies.
